
Our process
Our process
Free Intro
Schedule your free intro to discuss your goals, our services, and assess your current fitness.
Personalized Plan
We’ll tailor your workout plan based on your current fitness.
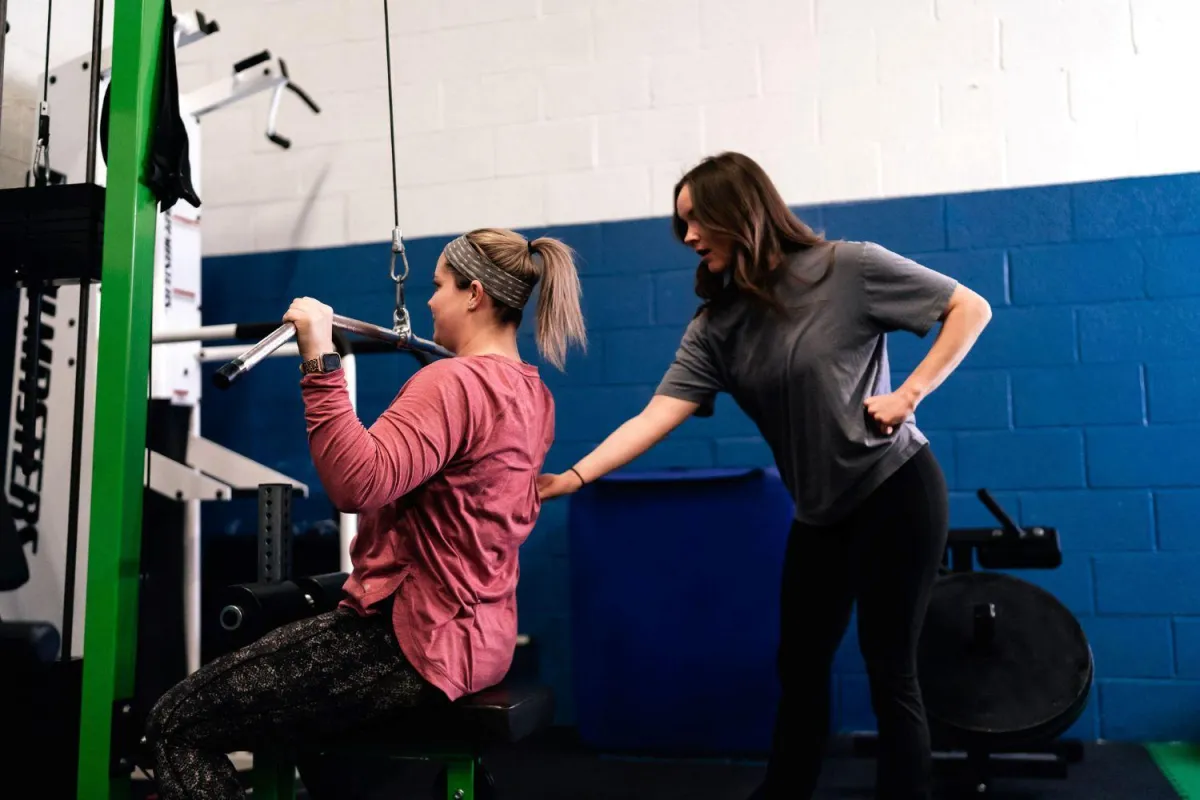
Results
With our attention to detail and science-backed programming, we deliver sustainable results.
Free Intro
Schedule your free intro to discuss your goals, our services, and assess your current fitness.
Personalized Plan
We’ll tailor your program to your current fitness, setting you up for
long-term success.
Results
With our attention to detail, science-backed programming and self-paced training sessions, we deliver sustainable results
experience the paragon difference
Tired of nagging injuries from random fitness programs, quick fixes that land you back at your starting point and navigating your health alone? Schedule your Free Intro to learn how we support you beyond a good sweat.
Our Programs

Semi-Private
Training
Personal training in a small group setting, with only four members per coach.
Personal
Training
Personal training is a one-on-one or partner experience.

Two Week
Trial
Not sure if Paragon is right for you? No sweat. We offer a two week trial for $49 so you can decide!
Hear it from our community

Address
Paragon Health & Fitness
19970 Ingersoll Dr.
Rocky River, OH 44116
Copyright © 2025 Paragon | All rights reserved | Designed By Zenplanner

